Comparing Influenza to COVID-19: A Public Health Perspective
Traversing the wide breadth of public health information available about SARS-CoV-2, which is the virus that causes the COVID-19 disease, has become increasingly difficult as data, and misinformation, have begun to accumulate. One common question is asked about similarities and differences between seasonal influenza (commonly, the flu) and COVID-19. While similarities between the two viruses do exist, there are some distinct differences that sets COVID-19 apart from influenza.
First, definitions of each virus will set the stage for discussing these similarities and differences. COVID-19 is an infection of the respiratory tract caused by a newly emergent coronavirus (SARS-CoV-2), which was first recognized in Wuhan, China, in December 20191. Influenza is a contagious respiratory illness caused by human influenza viruses. There are two main types of influenza virus, Type A and Type B, which are responsible for seasonal flu epidemics each year2.
Comparing Symptoms and Incubation Periods of COVID vs Flu
Common symptoms for both influenza and COVID-19 can include fever, cough, and fatigue. However, other symptoms like shortness of breath and respiratory issues seem to be more common with COVID-19 than with influenza. It is recommended by the Centers for Disease Control and Prevention (CDC) that development of symptoms including trouble breathing, persistent pain or pressure in the chest, confusion or the inability to fully awaken, and bluish lips or face constitute emergency warning signs of COVID-19, which may require immediate medical attention3. While symptoms are similar in adults and children4, a recent CDC Morbidity and Mortality Weekly Report suggested that fewer children than adults experience symptoms such as fever, cough, and shortness of breath5.
The incubation period for seasonal influenza is commonly one to four days, with most showing symptoms on the second day6. COVID-19 has an incubation period of one to 14 days7, although recent research suggests the median incubation period for COVID-19 is 5.1 days8. The period of contagiousness for influenza is generally one to seven days, meaning that a person without symptoms could potentially spread influenza one day before onset of symptoms, and up to seven days after becoming sick9. With COVID-19, there is not currently enough data to determine a period of contagiousness. However, a recent study observed that the median duration of viral RNA detection was 20 days10, and the longest observed duration of viral shedding was 37 days11,12.
Severity and Mortality of COVID-19 and Flu
Current data informs us that most people who contract COVID-19 will develop mild symptoms. However, approximately 14% - 16% of people will develop more severe illness which requires hospitalization and oxygen support, and of those, 5% will require admission to an intensive care unit13, 14. Older age and co-morbid diseases such as diabetes, hypertension, heart disease, and obesity, along with other disease-causing behaviors, such as smoking, are risk factors for increased mortality15,16.
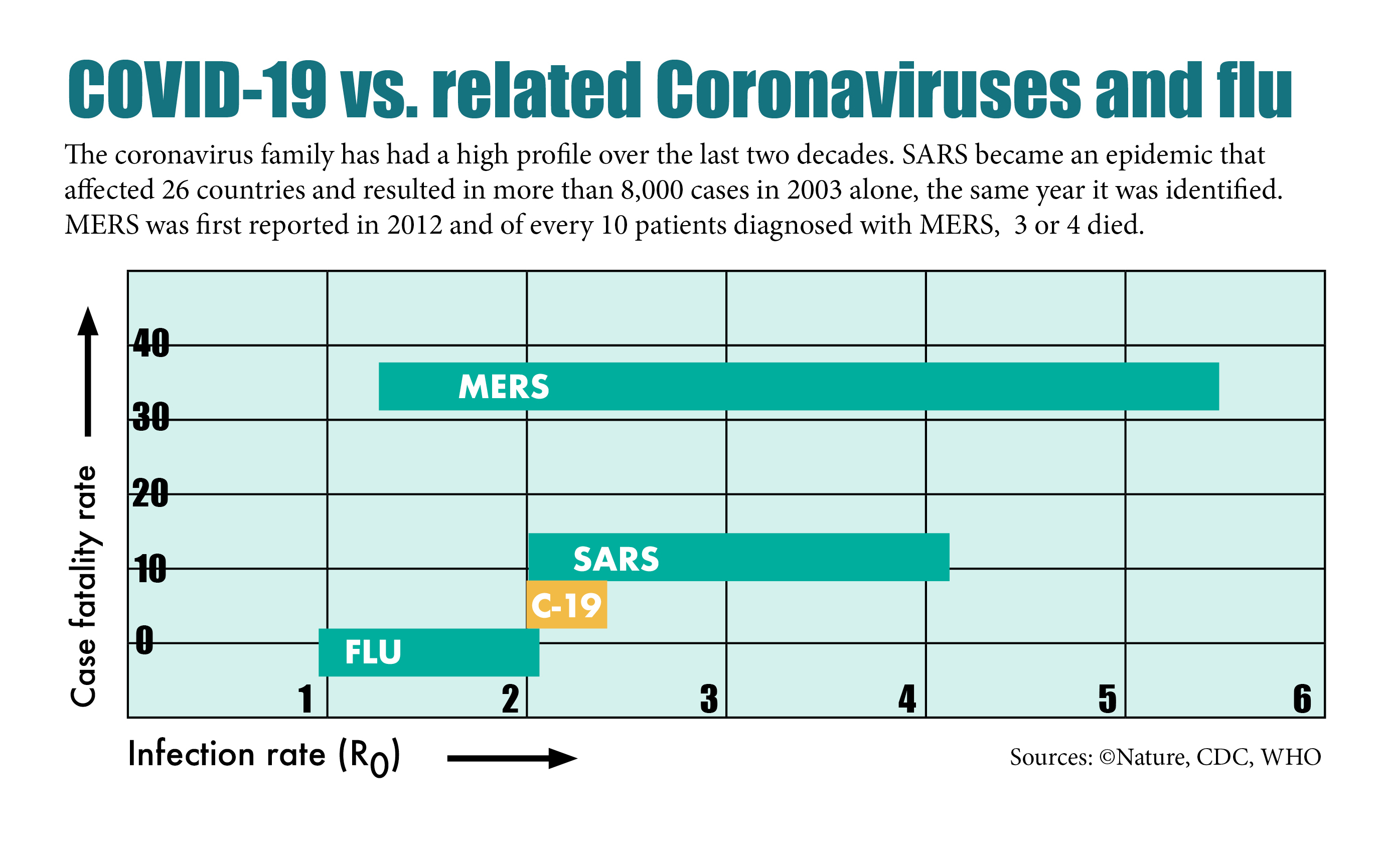
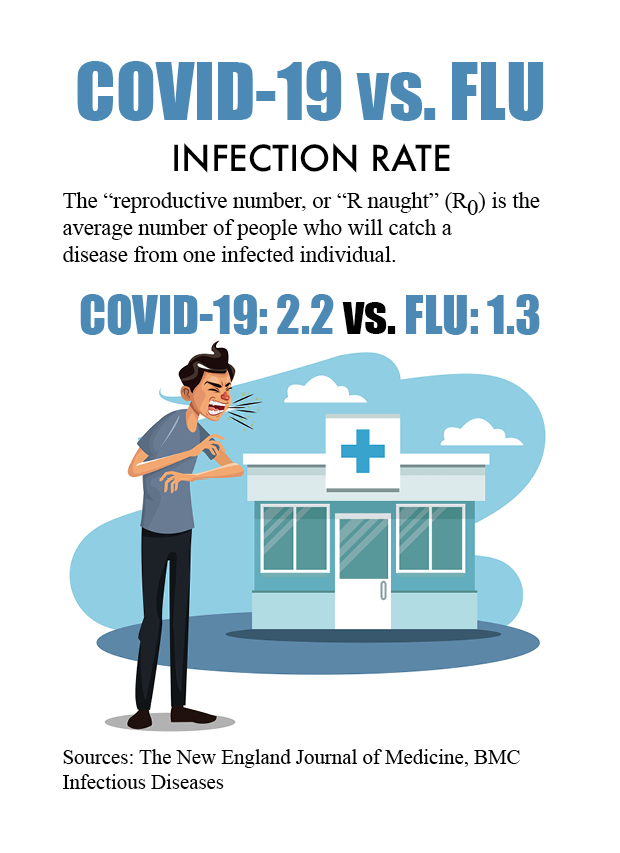
The reproductive number, or the average number of people who will catch a disease from one infected individual (sometimes referred to as R0, “R naught”) is useful for understanding how quickly a disease can spread. If
R0 is less than 1, each infected person will cause less than one new infection in another person. If R0 equals 1, each existing infection causes exactly one new infection in another person. However, if R0 is greater than 1, each infected person causes more than one new infection. In these cases, diseases spread between people, and may lead to an outbreak, epidemic, or pandemic, as we currently have with COVID-19. While we know that the R0 for influenza is estimated to be 1.3, a recent study estimates the R0 for COVID-19 to be 2.217,18. Compared to influenza, this means that each infected person with COVID-19 will infect up to 2.2 additional persons, leading, partially, to our current environment of a public health emergency. The graph below compares the R0 of COVID-19, and its case fatality rate, to other well-known communicable diseases27.
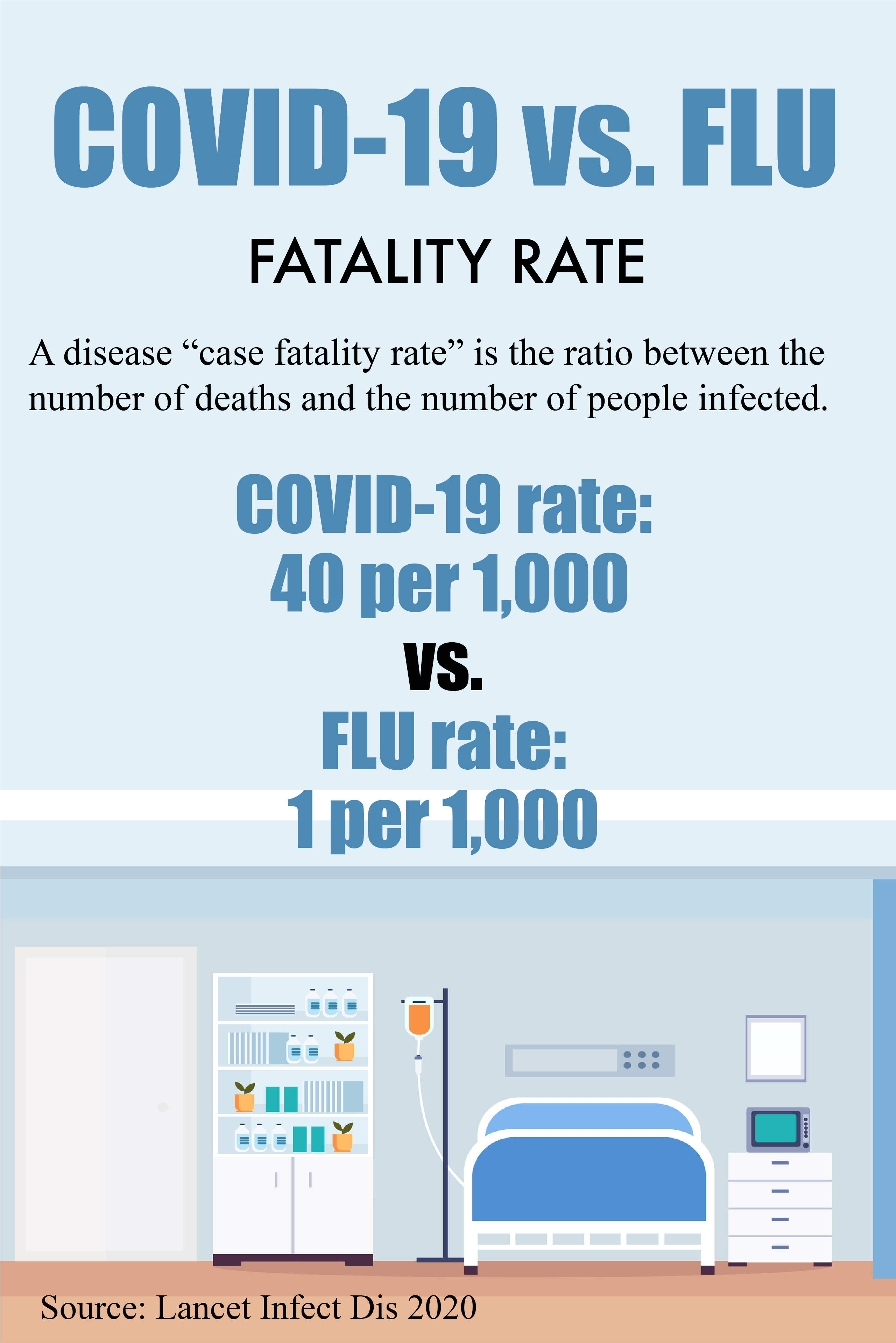
Based on recent data, the mortality rate for COVID-19 appears to be higher than for influenza. While it will take time to determine and fully understand the true mortality rate of COVID-19, present data from the World Health Organization (WHO) indicate a crude mortality rate (the number of reported deaths divided by the reported cases) of between 3-4%19. The WHO advises that the infection mortality rate (the number of reported deaths divided by the number of infections) will likely be lower. For influenza in the U.S., mortality is usually well below 0.1%. Known as the case fatality rate, seasonal influenza kills 1 in one-thousand (1:1,000) people that contract the virus as compared to COVID-19 that is projected to kill 40 people per thousand (40:1,000) infected with the virus14.
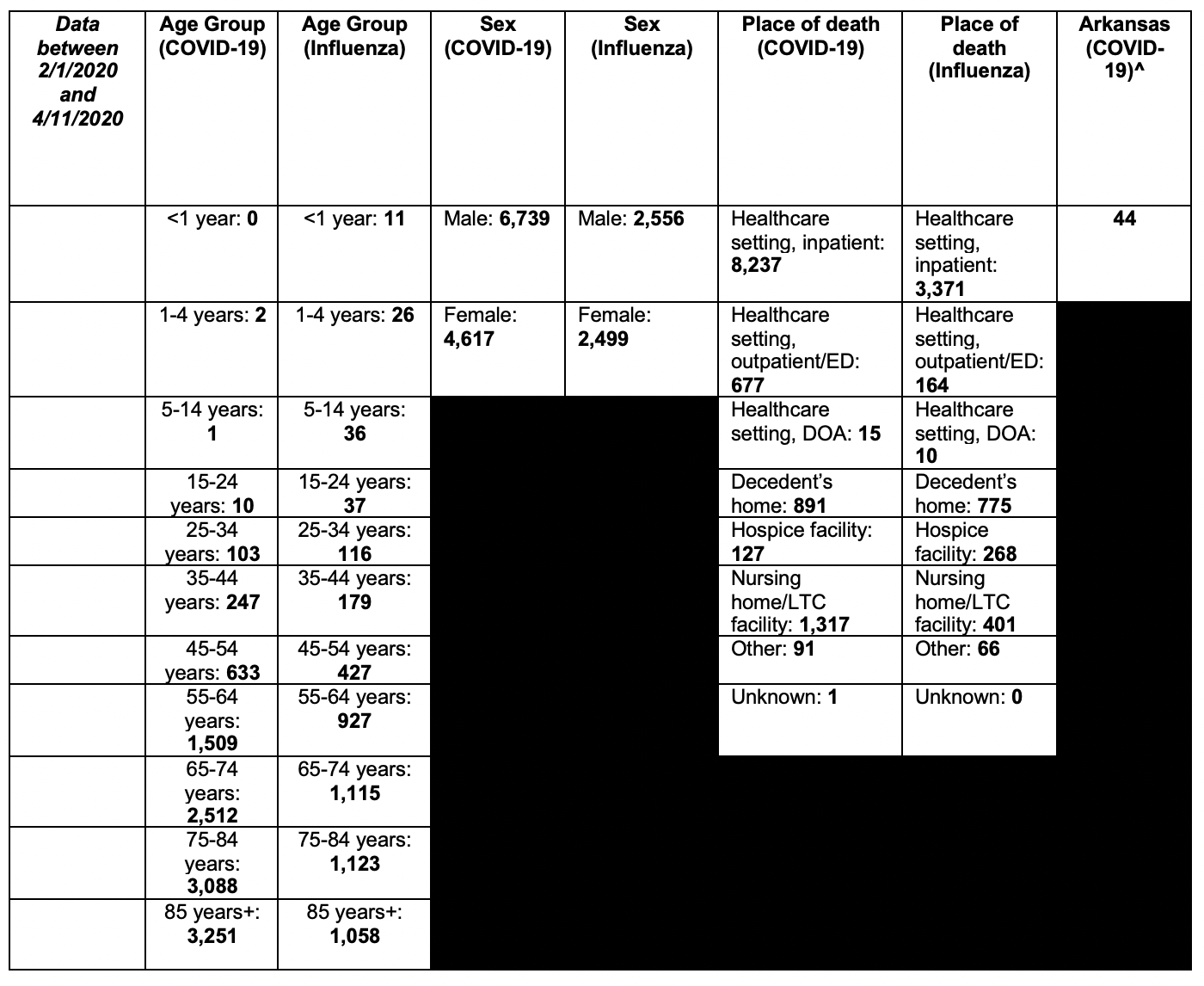
However, mortality rates will vary, as mortality is dependent upon and determined by access to and quality of health care19. Mortality rates and case rates also differ by geographic region, population density, age, gender, and environmental setting. Between the dates of February 1st and April 11th, 2020, the National Vital Statistics Systems reported 11,356 deaths in the United States, compared to 5,055 deaths attributable to influenza20.
Deaths involving coronavirus disease 2019 (COVID-19) and influenza to NCHS by age group, sex, and place of death
NOTE: Data during this period are incomplete because of the lag in time between when the death occurred and when the death certificate is completed, submitted to NCHS, and processed for reporting purposes. This delay can range from 1 week to 8 weeks or more, depending on the jurisdiction, age, and cause of death
^: Number of deaths for Arkansas come from the Arkansas Department of Health’s COVID-19 monitoring system, and are accurate as of 4/23/2020.
*To learn more about how the CDC categorizes provisional death counts from the National Vital Statistics System, please visit this website.
Hospitalization rates
Further, hospitalization rates among COVID-19 patients is approximately 16% of cases as compared to seasonal influenza rates at 0.68% of cases21. U.S. hospitals lack capacity to provide adequate care when rates of hospitalization increase dramatically over a short period of time. In testing the capacity of hospital bed and ventilator usage, researchers used the COVID-19 Hospital Impact Model (CHIME) under simulated conditions, which provides statistical data to estimate that hospital capacity for beds and ventilators may be exceeded by between 10% and 100% in a populated urban area22.
Preliminary data from 2018-2019 suggest that there were approximately 35.5 million cases of influenza in the United States, and approximately 34,000 deaths23. As of this writing, there are 1,914,916 confirmed cases of COVID-19 globally, with 123,010 deaths24. As of this writing, the United States has 605,390 confirmed cases of COVID-19, with 24,582 deaths25.
Note*: See Figures below for data visualization.
Transmission, Treatment, and Prevention
Like influenza, COVID-19 is spread from person to person primarily through respiratory droplets produced when an infected person coughs or sneezes. These droplets are then inhaled through the mouths or noses of others who are nearby. Both influenza and COVID-19 spread through “community spread,” meaning people have become infected with the virus by simply being near others who have the disease. People are thought to be most contagious when they are symptomatic, however, more recently the virus has also been detected in asymptomatic persons26.
Influenza has been a constant companion for humans for many decades, and therefore we are able to better treat and prevent influenza with symptom management, antiviral drugs, and even seasonal influenza vaccines. Currently, there are no approved treatments or vaccinations available to treat COVID-19. The current best practices include treating the symptoms and any co-morbid diseases that may occur along the disease trajectory.
Prevention tips
Preventing influenza, and especially preventing COVID-19, are current hot topics in public health, and each disease comes with its own set of prevention measures. First, the most effective way to prevent influenza is with an annual flu vaccine. At the time of this writing, no vaccine exists to prevent COVID-19, however. Instead, we can affect both influenza and COVID-19’s ability to spread and infect others by practicing non-pharmaceutical interventions (NPIs).
Non-pharmaceutical interventions include washing your hands often with soap and water for at least 20 seconds or using hand sanitizer that contains at least 60% alcohol if handwashing is unavailable; avoiding touching your eyes, nose, and mouth with unwashed hands; avoiding close contact with people who are sick, and relatedly, practicing social distancing by staying home as much as possible; covering your coughs and sneezes with a tissue, and then immediately washing your hands; cleaning and disinfecting frequently touched surfaces often, including tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks; and finally, wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies), especially in areas of significant community-based transmission, as is recommended by the CDC. Facemasks will help keep you from touching your nose and mouth, which prevents the spread of germs from your hands; protect your nose and mouth from large infected respiratory droplets from others’ coughs or sneezes; and, help keep others safe by limiting the transfer of infected respiratory droplets from your coughs and sneezes onto surfaces that others may touch.
For further information, and to help inform you about the constantly changing COVID-19 public health emergency, please visit https://www.uaex.uada.edu/covid19, the Centers for Disease Control and Prevention’s COVID-19 website, or the Arkansas Department of Health’s COVID-19 website.
References
- World Health Organization (WHO) (2020). Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. https://apps.who.int/iris/bitstream/handle/10665/331446/WHO-2019-nCoV-clinical-2020.4-eng.pdf?sequence=1&isAllowed=y
- Centers for Disease Control and Prevention (N.D.) Seasonal influenza: About flu. https://www.cdc.gov/flu/about/index.html
- Centers for Disease Control and Prevention (2020). Symptoms of coronavirus. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
- Centers for Disease Control and Prevention (2020). Frequently asked questions: COVID-19 and children. https://www.cdc.gov/coronavirus/2019-ncov/faq.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Fchildren-faq.html#COVID-19-and-Children
- Centers for Disease Control and Prevention (2020). Coronavirus disease 2019 in children—United States, February 12-April 2, 2020. Morbidity and Mortality Weekly Report 69(14): 422-426. https://www.cdc.gov/mmwr/volumes/69/wr/mm6914e4.htm
- Centers for Disease Control and Prevention (2018). Seasonal influenza: How flu spreads. https://www.cdc.gov/flu/about/disease/spread.htm
- World Health Organization (WHO). (2020). Q&A on coronavirus (COVID-19). https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
- Laurer, S., Grantz, K., Bi, Q., Jones, F., Zheng, Q., Meredith, H., et al. (2020). The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Annals of Internal Medicine. doi: 10.7326/M20-0504. https://annals.org/aim/fullarticle/2762808/incubation-period-coronavirus-disease-2019-covid-19-from-publicly-reported
- Centers for Disease Control and Prevention (2018). Seasonal influenza: How flu spreads. https://www.cdc.gov/flu/about/disease/spread.htm
- Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020. Epub 2020/02/28. doi: 10.1016/S2213-2600(20)30079-5. PubMed PMID: 32105632. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30079-5/fulltext
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. Epub 2020/01/28. doi: 10.1016/S0140-6736(20)30183-5. PubMed PMID: 31986264. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30183-5/fulltext
- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective study. Lancet, 2020. doi: 1016/S0140-6736(20)30566-3. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30566-3/fulltext
- Team NCPERE. Vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) – China. China CDC Weekly. 2020;2(8):113-22. https://www.ncbi.nlm.nih.gov/pubmed/32064853
- Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020; published online Feb 19. https://doi.org/10.1016/S1473-3099(20)30120-1.
- Guan, W. J., Liang, W. H., Zhao, Y., Liang, H. R., Chen, Z. S., Li, Y. et al. & China Medical Treatment Expert Group for Covid-19 (2020). Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis. The European respiratory journal, 2000547. Advance online publication. https://doi.org/10.1183/13993003.00547-2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7098485/
- Centers for Disease Control and Prevention (2020). Coronavirus Disease 2019 (COVID-19): Information for people who are at higher risk for severe illness . https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/
- Biggerstaff, M., Cauchemez, S., Reed, C., Gambhir, M., & Finelli, L (2014). Estimates of the reproduction number for seasonal, pandemic, and zoonotic influenza: A systematic review of the literature. BMC Infectious Diseases, 14: 480. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4169819/pdf/12879_2014_Article_3799.pdf
- Qun, L., Guan, X., Wu, P., Wang, X, Zhou, L., Tong, Y., et al. (2020). Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. The New England Journal of Medicine, 382(13): 1199-1207. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7121484/
- World Health Organization (WHO) (2020). Coronavirus disease 2019 (COVID-19) Situation Report—46. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200306-sitrep-46-covid-19.pdf?sfvrsn=96b04adf_2
- Centers for Disease Control and Prevention (2020). National Center for Health Statistics, National Vital Statistics System: Provisional death counts for coronavirus disease (COVID-19). https://www.cdc.gov/nchs/nvss/vsrr/COVID19/index.htm
- Centers for Disease Control and Prevention (2020). Seasonal Influenza (Flu): Weekly U.S. Influenza Surveillance Report.
- Weissman GE, Crane-Droesch A, Chivers C, et al. Locally Informed Simulation to Predict Hospital Capacity Needs During the COVID-19 Pandemic. Ann Intern Med. 2020; [Epub ahead of print 7 April 2020]. doi: https://doi.org/10.7326/M20-1260
- Centers for Disease Control and Prevention (2020). Seasonal Influenza (Flu): Disease Burden of Influenza. https://www.cdc.gov/flu/about/burden/index.html
- World Health Organization (WHO) (2020). Coronavirus disease 2019 (COVID-19) Situation Report—85. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200415-sitrep-86-covid-19.pdf?sfvrsn=c615ea20_2
- Centers for Disease Control and Prevention (2020). Coronavirus Disease 2019 (COVID-19): Cases in U.S. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
- Centers for Disease Control and Prevention (2020). Coronavirus Disease 2019 (COVID-19): How COVID-19 spreads. https://www.cdc.gov/coronavirus/2019-ncov/faq.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Fchildren-faq.html
- Callaway, E., Cyranoski, D., Mallapaty, S., Stoye, E., & Tollefson, J. (2020). The coronavirus pandemic in five powerful charts. Nature, 579:482-483. https://www.nature.com/articles/d41586-020-00758-2
Figures
Figure 1
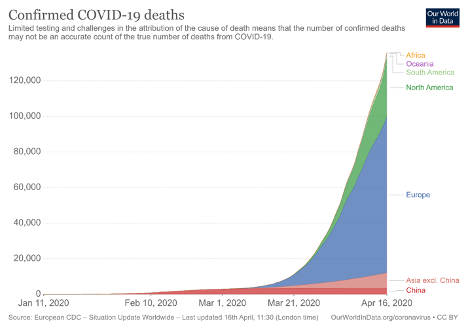
Figure 2
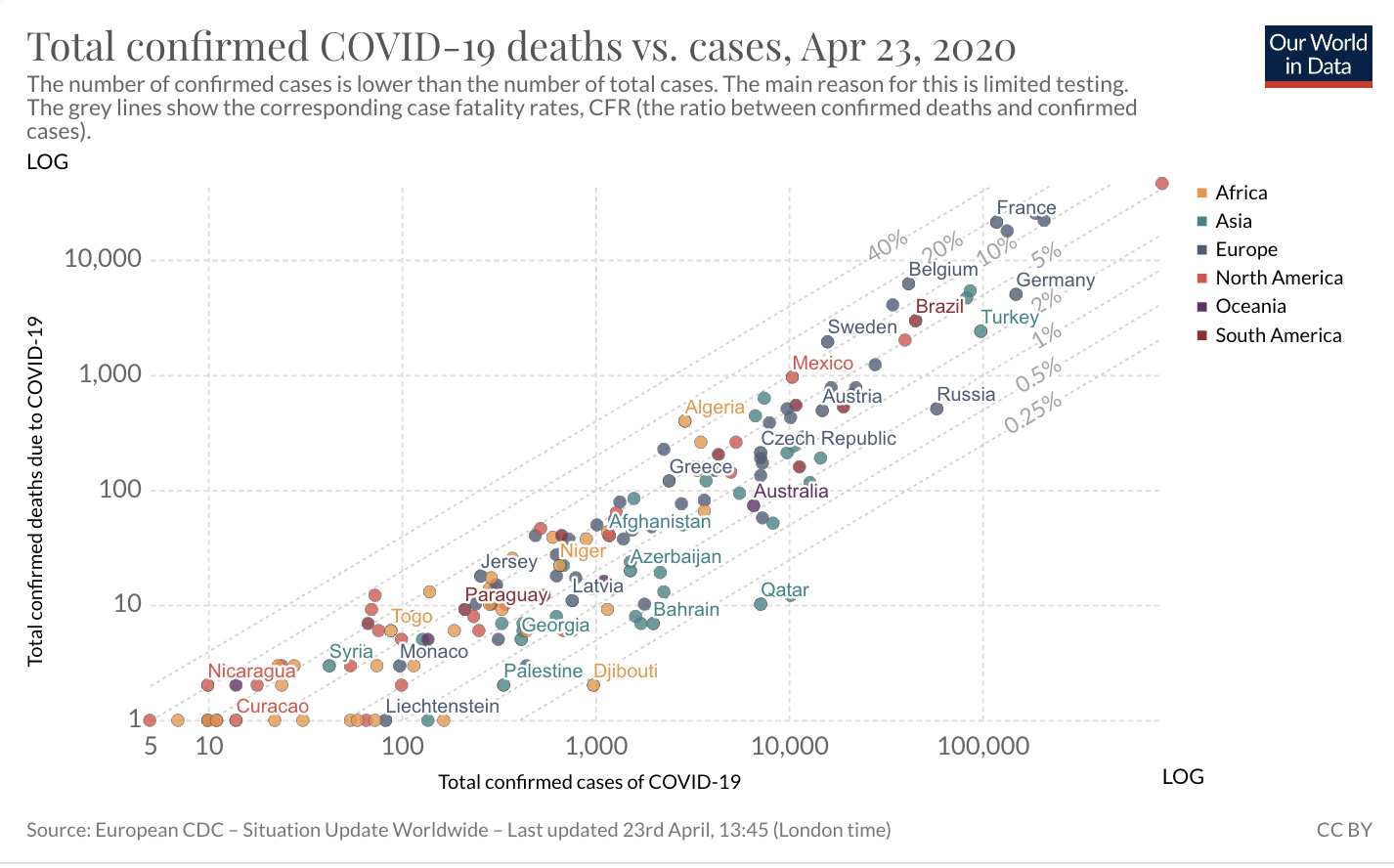
Figure 3
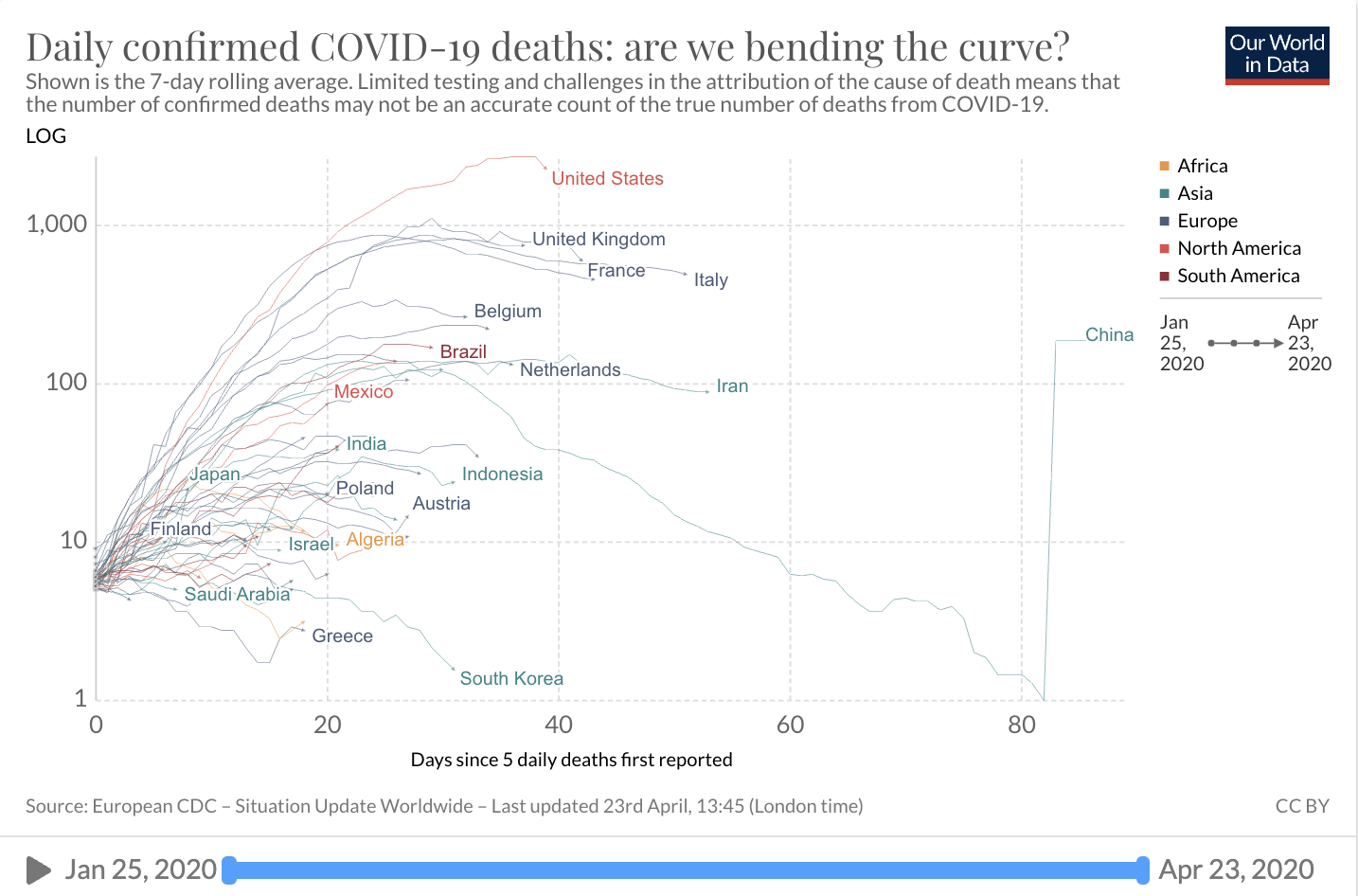
Figure 4
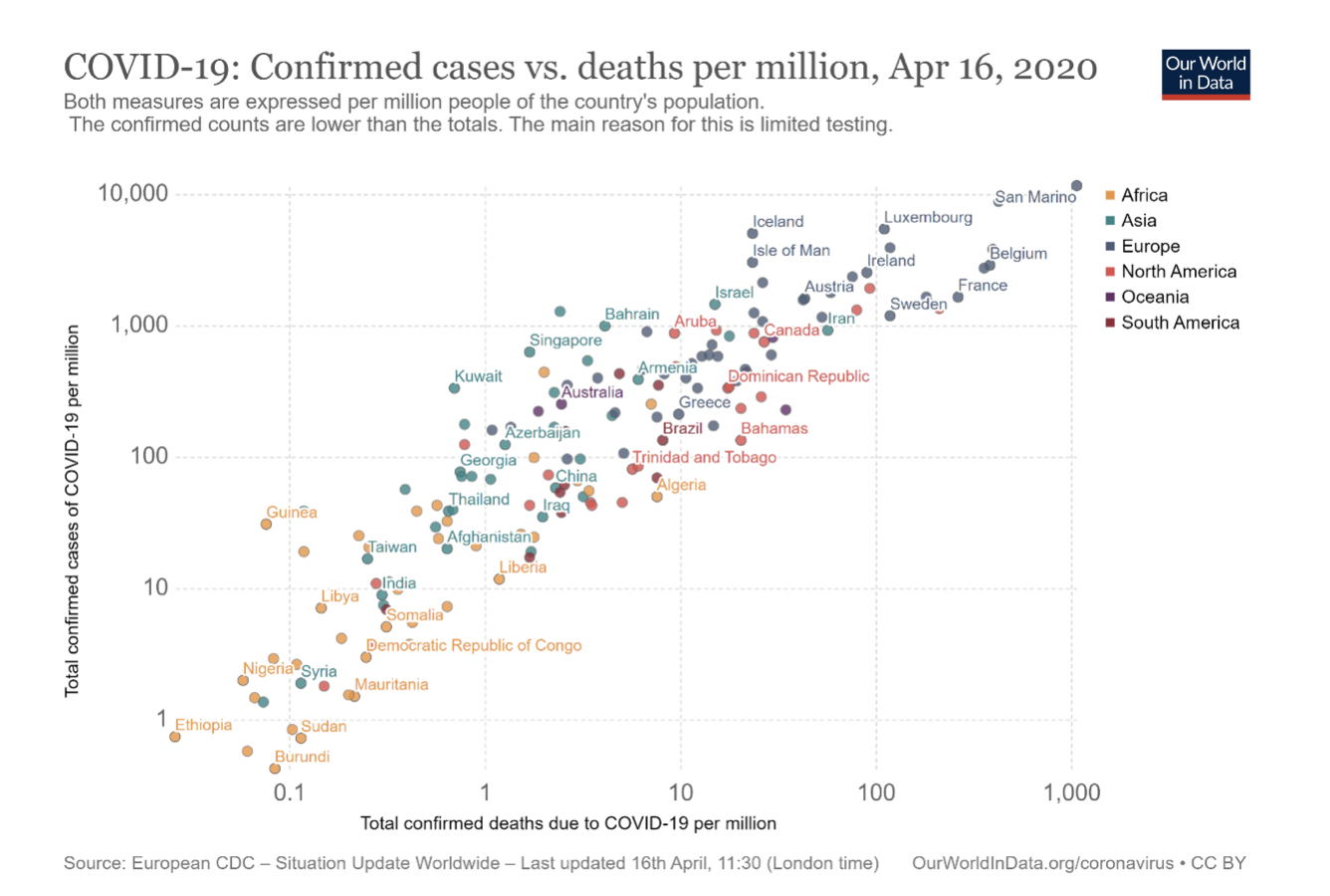
Data visualizations can be found here and here.
Contact Dr. Mader: