Posts
Contact
Frank Seo
CPED
Phone: 501-671-2083
Email: fseo@uada.edu
University of Arkansas System Division of Agriculture
Cooperative Extension Service
2301 S. University Avenue
Little Rock, AR 72204
Connecting Health and Economic Growth in Rural Arkansas
We explore how improving health and economic growth go hand in hand in rural Arkansas, highlighting data, disparities, and strategies for resilient communities.
The Vital Link Between Health and Economic Prosperity
Public health and economic development are two sides of the same coin. A strong economy supports public health by providing resources for education, employment, healthcare and infrastructure. In turn, healthy communities drive economic growth through a productive workforce, higher labor participation and reduced healthcare costs.
As the 2021 U.S. Department of Health and Human Services report Community Health and Economic Prosperity notes, “We cannot have healthy communities without a prosperous economy, and we cannot have a prosperous economy without healthy communities.”
This interdependence is especially evident in rural Arkansas, where health disparities and economic challenges are closely linked.
The Health-Economy Connection in Arkansas
The 2025 Rural Profile of Arkansas reveals that health and economic challenges are deeply interconnected, threatening the sustainability of rural communities. Figure 1 shows Health Factor scores from The Robert Wood Johnson Foundation’s County Health Rankings. This composite score measures health-related behaviors, clinical care, social and economic factors, and quality of the physical environment, with a higher score representing less favorable conditions for health outcomes.
Many rural counties, particularly in the Delta and Coastal Plains regions, show higher Health Factor scores, signaling unfavorable conditions for health. These issues are further compounded by high infant mortality rates, poor maternal health outcomes, food insecurity and widespread obesity. Meanwhile, continued shortages of nurses and physicians, especially in remote counties, limit access to care and place additional strain on local health systems (GlobalData Plc, 2023).
Figure 1. Health Factor Scores, 2024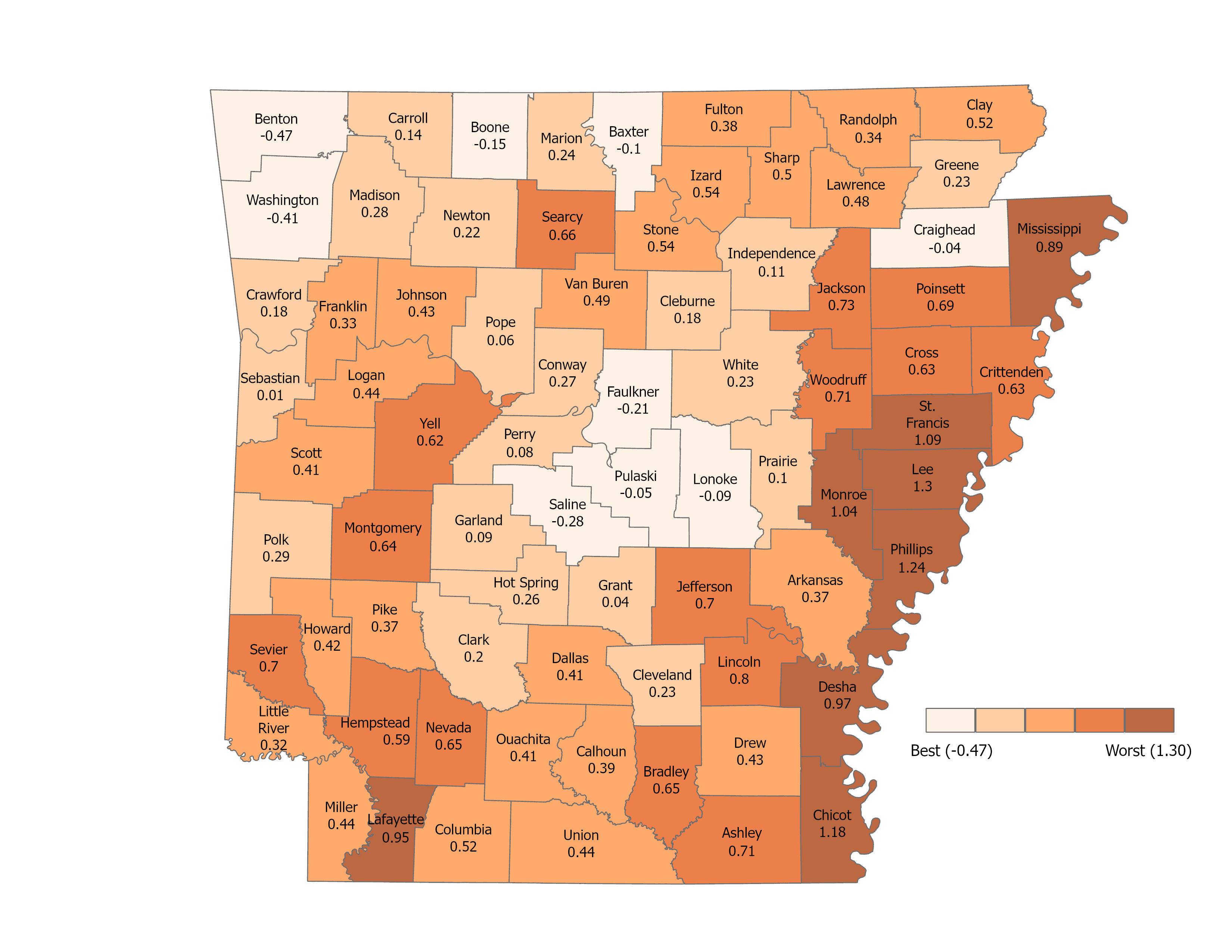 Source: 2025 Rural Profile of Arkansas, University of Arkansas System Division of
Agriculture
Source: 2025 Rural Profile of Arkansas, University of Arkansas System Division of
Agriculture
Furthermore, Figure 2 illustrates the close relationship between health and employment trends in rural Arkansas. Counties with high Health Factor scores, such as Phillips, St. Francis and Monroe in the Delta region, experienced a net loss of jobs between 2013 and 2022. In contrast, counties in and around urban regions—northwest Arkansas (Washington and Benton), central Arkansas (Saline and Faulkner), and northeast Arkansas (Craighead)—saw net employment gains and typically demonstrate more favorable health conditions. This pattern highlights how economic vitality and community health reinforce one another, shaping the long-term resilience of rural communities.
Figure 2. Percent Change in Employment Between 2013 and 2022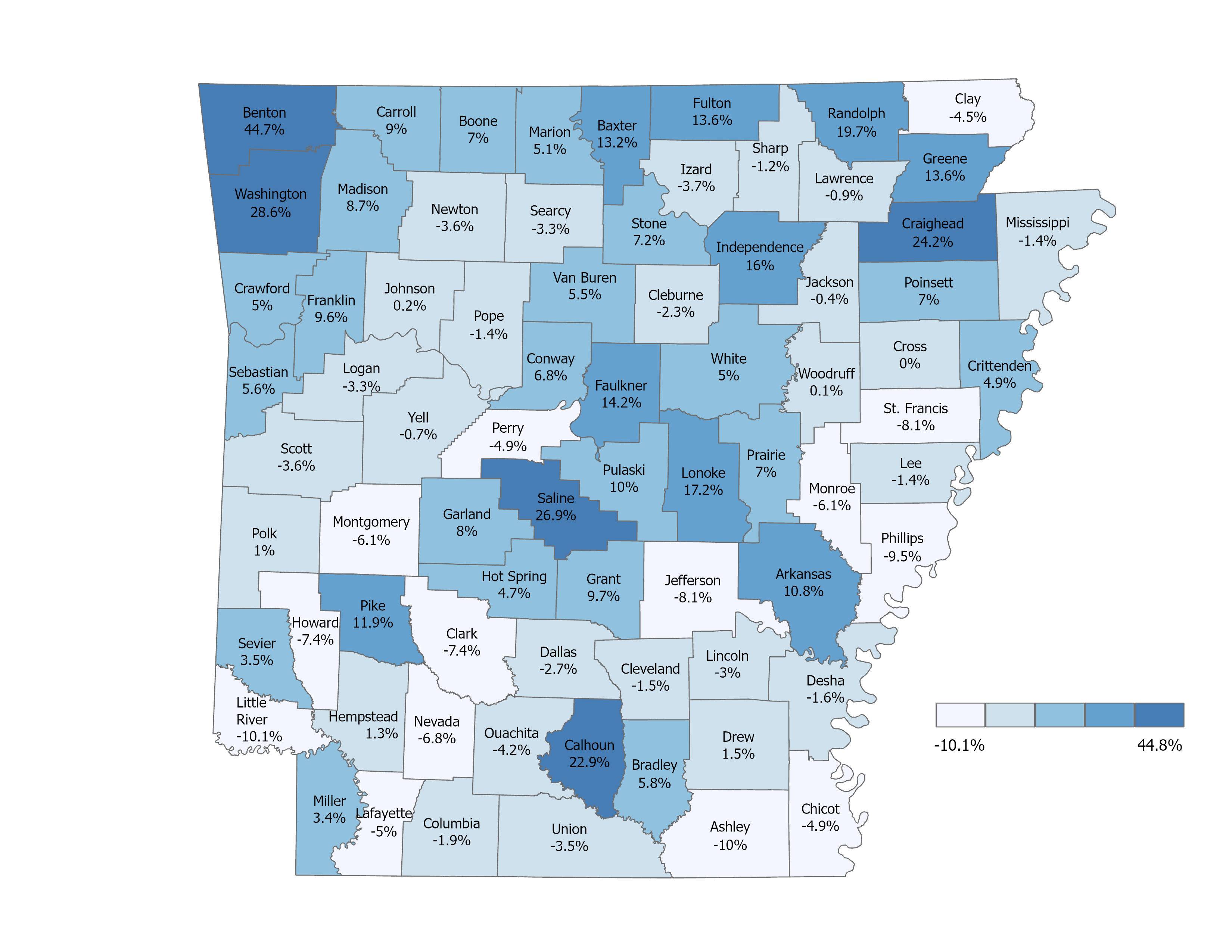 Source: 2025 Rural Profile of Arkansas, University of Arkansas System Division of
Agriculture
Source: 2025 Rural Profile of Arkansas, University of Arkansas System Division of
Agriculture
Integrating Public Health into Economic Development in Rural Arkansas
Many rural counties face limited budgets, aging infrastructure, and small populations, making it difficult to fund new healthcare initiatives, community projects, or attract business investment. These constraints highlight the need for a holistic approach, one that integrates health equity into economic development planning. Strengthening this connection is essential for building resilient and sustainable rural economies. Therefore, communities can adopt several strategies to simultaneously improve public health and stimulate economic prosperity:
- Food Systems Planning: Expanding access to affordable, nutritious foods is essential for promoting healthier
lifestyles. Strategies such as establishing Food Policy Councils (FPCs), raising asset
limits for SNAP benefits, deploying mobile food hubs and pantries, supporting food
delivery models, and enacting fiscal policies that promote food access (e.g., local
tax incentives, revolving loan programs, and grant funds) can help improve food security
in distressed communities (Arkansas Hunger Relief Alliance, 2022; Oza-Frank et al.,
2025).
- Built Environment Improvements: Developing complete streets, bike trails, parks, and open spaces encourages physical
activity and enhances community well-being (Blum, 2014).
- Healthcare Workforce Development: Addressing workforce shortages through career pathways, training programs, stipends,
and incentive packages can strengthen healthcare capacity. Tackling root causes of
turnover, such as burnout, housing shortages, and limited community amenities, is
also critical (GlobalData Plc, 2023).
- Support Funding for Rural Hospitals: Establishing a national minimum for the Medicare Area Wage Index could help reduce
disparities in hospital payment rates between rural and urban areas, strengthening
rural healthcare infrastructure (GlobalData Plc, 2023).
- Enhance Cross-Sector Coordination: Improved coordination and data sharing between public health and economic development sectors are essential for tracking progress and ensuring policies complement one another.
Realistic Challenges and Next Steps
Implementing these strategies often depends on broader structural and technological support. Policy changes, such as updating the Medicare Area Wage Index or SNAP eligibility, require government backing and can take time. Similarly, effective coordination between health and economic sectors relies on technology that many rural areas currently lack. Despite these challenges, progress is possible. Small, incremental steps through grants, business partnerships, and community-led initiatives can gradually improve health outcomes while stimulating economic growth.
References
Arkansas Hunger Relief Alliance. (2022). Arkansas Governor’s Food Desert Working Group report. https://arhungeralliance.org/wp-content/uploads/2022/12/Food-Desert-Working-Group-Report.22.pdf
Blum, E. S. (2014). Healthy communities: A framework for meeting CRA obligation. Federal Reserve Bank of Dallas. https://www.dallasfed.org/cd/healthy/~/media/documents/cd/healthy/CRAframework.pdf
GlobalData Plc. (2023). Arkansas health workforce projections: 2021–2035. Arkansas Hospital Association. https://www.arkhospitals.org/images/webdocs/ArkansasWorkforceReport-January2023.pdf
Oza-Frank, R., Warnock, A. L., Calancie, L., Bassarab, K., Palmer, A., Cooksey Stowers, K., … & others. (2025). Food policy councils and healthy food access policies: A 2021 national survey of community policy supports. Preventing Chronic Disease, 22, Article 240335. https://doi.org/10.5888/pcd22.240335
Seo, F., & Goodman, M. (2025). 2025 Rural Profile of Arkansas. University of Arkansas System Division of Agriculture.
U.S. Department of Health and Human Services. (2021). Community health and economic prosperity: Engaging businesses as stewards and stakeholders—A report of the Surgeon General. Centers for Disease Control and Prevention, Office of the Associate Director for Policy and Strategy.